In London’s Great Ormond Street Hospital, two young teenagers were about to be discharged. Each had cystic fibrosis, a genetic condition that causes mucus to build up in the lungs. Recently, both had been fortunate enough to receive double-lung transplants, which can provide relief from some of the breathing problems associated with their condition.
For many, the surgery is a lifesaver. But for the patients in London, the transplants had initiated a set of new, life-threatening problems.
Transplants require heavy doses of drugs that suppress the immune system so that patients’ bodies don’t reject the new organs, but those same drugs also leave the body susceptible to infections. In the wake of their surgeries, the two teens got sick, and then sicker. The culprit: superbugs, bacteria that have evolved to become resistant to antibiotics.
As medical options dwindled, the doctors were forced to switch the patients’ treatment plans to in-home palliative care, which focuses on managing pain and discomfort. Essentially, they were being sent home to die. It was just before Christmas 2017.
But there was still one longshot treatment possibility. The doctors knew of a researcher an ocean away at the University of Pittsburgh who might just hold the key to saving the teenagers’ lives.
Graham Hatfull, Pitt’s Eberly Family Professor of Biotechnology, is a phage expert. Most people haven’t heard of phages, short for bacteriophages, but there are approximately 10 million trillion trillion of them, or about 10 million more than there are stars in the universe.
“Phage particles are the majority of all biological stuff on the planet,” Hatfull says.
Under an electron microscope, they look like lunar landers crossed with robot spiders. In essence, they are viruses that use bacteria to reproduce. Some phages, known as virulent phages, hijack a bacterial cell’s machinery to create copies of themselves. They then multiply inside bacteria until there are so many that they burst out like candy from a smacked piñata. The bacteria die as a result, and each new phage goes on the prowl for more hosts in which it can repeat the process. It’s fitting that “phage” comes from the Greek word phágos, “a thing that devours.”
The London doctors wondered whether Hatfull knew of phages that could combat the bacteria infecting their patients.
Phage therapy, as it is called, isn’t new. The technique was first discovered in 1915 at the Pasteur Institute in France, but it mostly fell out of favor with the rise of antibiotics.
The therapy is problematic because phages are picky eaters. Each one has evolved into a highly specialized predator of usually just one specific kind of prey. That’s why even though phages are everywhere, they can’t simply be grabbed from a puddle and injected into a sick person. Doctors need someone who can find precisely the right phage for the job.
Enter Hatfull. He and his team at Pitt are among the world’s leaders in collecting phages and learning what they do. In 2002, Hatfull helped develop the Phage Hunters Integrating Research and Education (PHIRE) program with support from the Howard Hughes Medical Institute. Through PHIRE, Pitt undergraduates with an interest in research processed soil samples in the hopes of discovering new phages. They then learned to describe the viruses, gave them unique names, and entered them into an ever-growing database.
In 2006, as Hatfull refined the phage-hunting framework, the program grew into a global network called Science Education Alliance–Phage Hunters Advancing Genomic and Evolutionary Science (SEA-PHAGES), which is an undergraduate program that teaches science students the process of discovering phages. More than 25,000 students at 150 schools from Nigeria to New Zealand have participated, including hundreds from Pitt, helping to collect thousands of new-to-science phages. Beyond discovery, students learn advanced scientific techniques, including DNA sequencing and analyses of gene function by categorizing the phages. As lead scientist for SEA-PHAGES, Hatfull sets the international program’s overall goals.
Could any of those SEA-PHAGES discoveries devour the bacteria killing the two teenagers in London? Hatfull wasn’t sure. He had never looked for phages to fight an infection in a living person before. But he would try.
When the patients’ bacteria strains arrived from London in November 2017, Hatfull and his lab got to work. “We not only screened our collection,” Hatfull recalls, “but we also tried isolating phages from the environment that might be good candidates.”
Amazingly, in late January 2018, the team isolated a phage from a mixture of mud and animal droppings that appeared to attack the strain of bacteria afflicting one of the patients. Yet, as the cultures grew in petri dishes on the Pittsburgh campus, a process that can take several weeks, the worst happened: The patient died.
 The remaining patient, Isabelle, was 15 years old. With the antibiotic-resistant bacteria still wreaking havoc throughout her body, her liver had begun to fail.
The remaining patient, Isabelle, was 15 years old. With the antibiotic-resistant bacteria still wreaking havoc throughout her body, her liver had begun to fail.
To find the ideal phage therapy mix was an unprecedented challenge for Hatfull, who has been working with phages for decades. He earned his PhD in 1981 at Scotland’s University of Edinburgh and completed postdoctoral studies at Yale University before joining Pitt’s Department of Biological Sciences in 1988. Early in his research career, he says he considered phages as mere tools he could use to study more interesting facets of microbiology. But, in time, he became fascinated with the phages themselves because they’re abundant, easy to manipulate, and sources of potential genetic and molecular tools for fighting infections.
In 1988, he began sequencing the genome of a mycobacteriophage named L5. It took him five years. At the time, he thought it would be the only phage genome he’d ever sequence, but 26 years later, he and his team have sequenced more than 1,800 phages. All of that nitty-gritty genetic information has led to the creation of a phage family tree, based on which viruses are most closely related to each other.
For Isabelle’s case, Hatfull’s lab manager, Carlos Guerrero (GSPH ’14), and research associate, Rebekah Dedrick, delved into that family tree searching for candidates whose sequencing best meshed with Mycobacterium abscessus, the strain of bacteria inside Isabelle.
Once they identified a possible match, they went to the lab’s freezer, withdrew a vial of the preserved phage, and pitted it against a sampling of Isabelle’s bacteria for petri dish combat. If the cloudy dish of microbes cleared, the team would know they had found a bacteria killer. The team was hopeful but hardly optimistic. They were in for a surprise.
“We actually found one!” Dedrick remembers exclaiming upon viewing the dish.
The phage, named Muddy, was discovered in 2010 by Lilli Holst, a student participating in a SEA-PHAGES-like course at the University of KwaZulu-Natal in South Africa. According to the database notes, Holst found Muddy in a compost bin, on the underside of a rotting eggplant.
There was no time for celebration, though. Phages and bacteria have been at war forever, making them adept at defeating each other. If Hatfull’s team sent only Muddy to London, it was likely Isabelle’s infection would develop a resistance, just as it did with antibiotics. To give the treatment the best chance for success, a cocktail of phages would be needed, each from a different part of the family tree, making it harder for the bacteria to defend itself.
Dedrick and Guerrero had to make lightning strike not just once, but three times.
Years before, in summer 2006, Pitt undergraduate Tim Sampson volunteered to be a Hatfull phage hunter. His search took him to sites not on campus tours—moist, dirty settings where bacteria might prosper, because where bacteria go, phages follow.
Knowing that, he snatched a piece of debris from a storm drain outside of Heinz Memorial Chapel. Back at Hatfull’s lab, he used microbiology techniques to first isolate a phage from the muck and then watch it go toe-to-toe against bacteria in a petri dish. During his studies at Pitt, Sampson uncovered its genetic sequence. He christened the virus BPs—for Basement Productions, in homage to his high school theater group.
Sampson went on to earn his PhD in microbiology and molecular genetics at Emory University, where he now conducts his own research program. He credits his experience phage-hunting with Hatfull as a crystallizing factor in his decision to become a researcher. These days, he studies how the microbiome contributes to neurological conditions such as Alzheimer’s and Parkinson’s. He hasn’t thought much about BPs since graduating from Pitt in 2008.
“While we always discussed phage therapy as a possibility, it always seemed so far down the line,” Sampson says.
Twelve years down the line, as it turned out. In January 2018, Hatfull’s team identified BPs as a second phage that could go into Isabelle’s therapeutic cocktail. More shouts of joy! More work ahead.
Weeks passed. Petri dishes were prepped, incubated, and discarded.
In February 2018, with time running out for Isabelle, Dedrick and Guerrero plucked another compatible virus out of the abyss. This one, named ZoeJ, had been discovered in 2012 by Seth Pinches, a Providence College student. He had isolated the phage from rocky soil beneath a tree with red berries. Pinches named the phage after his baby niece, Zoe Jean.
The elation in the lab was palpable, but not without angst, too. Even with three phages, there remained a grave concern. Virulent phages kill bacterial cells by taking over their guts and then making the microbes explode, but there are also temperate phages, which reproduce by sneaking inside bacteria and altering their DNA—a less effective process for phage therapy.
 The first phage, Muddy, is virulent, and therefore was ready to destroy Isabelle’s bacteria; but BPs and ZoeJ are temperate and were not a sure thing for overcoming Isabelle’s infection.
The first phage, Muddy, is virulent, and therefore was ready to destroy Isabelle’s bacteria; but BPs and ZoeJ are temperate and were not a sure thing for overcoming Isabelle’s infection.
Hatfull, relying on his knowledge from his years of research and experience, made a bold decision. His team would remove a repressor gene in BPs and ZoeJ that would free them of their temperate lifestyle and unleash their inner bacteria-bursting beasts. These sorts of modifications are common in labs for research purposes, but nobody had ever injected a genetically modified phage into a person.
“We were in uncharted territory,” Hatfull says.
The team agonized over every detail, every pitfall that might lead to disaster. What if the phages did their job, for instance, but the dying bacteria released a substance that would prove toxic to Isabelle? “That’s the stuff that keeps you awake at night,” Hatfull says.
Before the treatment was approved, a rigorous regulatory process had to be completed. Hatfull and his team did their due diligence through various testing and scouring of scientific literature for any cases that might lend insight. But when you’re the first to try something, you can’t find answers to all of the “what ifs.”
“You worry,” Hatfull admits. “There were a lot of unknowns.”
In the seven months that had passed since her lung transplant, Isabelle’s incision continued to weep with fluids and had become flame-red around its edges. Sores had broken out on her arms, legs, and buttocks. Inside her body, Isabelle’s liver struggled to filter toxins from her blood while her new lungs filled up with the superbug bacteria.
Phage therapy was her last hope, the doctors agreed; with her parents’ consent, they scheduled her treatment. Dedrick flew to London the day before to monitor Isabelle’s blood, skin, and fecal samples to determine what was happening throughout Isabelle’s body.
“On the plane ride over there, I remember thinking, this could be really bad,” Dedrick recalls. “Because it was the first time, we didn’t know what to expect.”
Isabelle’s medical team—led by Helen Spencer, the hospital’s respiratory pediatrician and clinical lead for lung transplant services—decided to err on the side of caution and test the phage therapy on the external wounds first, using a topical solution.
Hours passed, and thankfully Isabelle’s body showed no signs of rejection. Reasonably satisfied that it was safe to proceed, Spencer had an IV drip the phages into Isabelle’s veins. The wait began, with Isabelle’s life hanging in the balance.
“Almost overnight, things started to clear up and heal,” a grateful Jo Holdaway, Isabelle’s mother, told CNN about the case that captured worldwide attention. “It was just amazing.”
In six more weeks, Isabelle’s infection nearly disappeared. The phages did what the antibiotics couldn’t.
 Today, more than a year since the June 2018 treatment, Isabelle still receives phage therapy on a regular basis, but her microbe levels are so low and her breathing so improved that she is no longer bedridden. She’s returned to school and in many ways is living a normal, teenage life.
Today, more than a year since the June 2018 treatment, Isabelle still receives phage therapy on a regular basis, but her microbe levels are so low and her breathing so improved that she is no longer bedridden. She’s returned to school and in many ways is living a normal, teenage life.
Hatfull is deeply proud of his team.
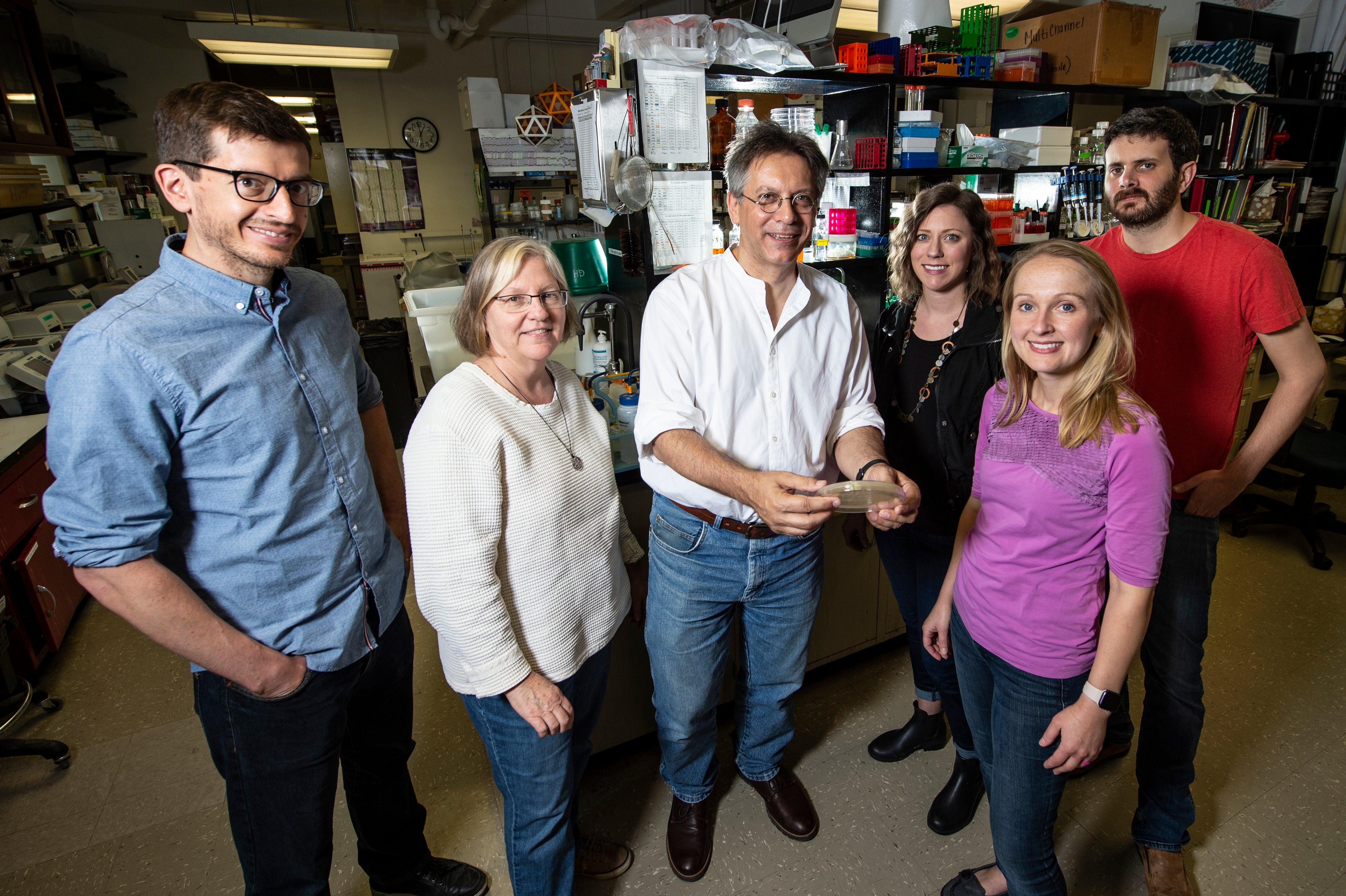
“These guys are really good,” he says, pointing out that it was Guerrero and Dedrick who found the phages; Rebecca Garlena (A&S ’07) and Daniel Russell who oversaw the DNA sequencing; and Deborah Jacobs-Sera (SHRS ’77, EDUC ’98G) who carried out the therapeutic phage preparations. And, of course, there’s the vast international network of student scientists whose hands-on learning with SEA-PHAGES over the years helped create a catalog of phages that has proved invaluable.
However, the thrill over Isabelle’s outcome is tempered by the tragedy of losing the other patient. The researchers in Hatfull’s lab are used to working behind the bench, not at the bedside. This brush with life and death isn’t what they initially expected from their academic careers.
“It’s sobering,” Hatfull says. “We haven’t had to deal with those issues and now that becomes very real.”
In May 2019, Hatfull and Spencer published the details of Isabelle’s case in one of the world’s most highly regarded medical journals, Nature Medicine. Their work marked the first therapeutic use of engineered phages and the first known attempt to use phages to treat a mycobacterial infection in a human. Although the scientists emphasize that there is still much to learn, the results excited many experts.
Steffanie Strathdee, codirector of the University of California San Diego’s Center for Innovative Phage Applications and Therapeutics and author of The Perfect Predator, a memoir about the successful search for phages to cure her husband of a superbug, says it was “ingenious” for Hatfull’s team to use genetically modified phages. “I think it’s really the way of the future, because it makes it easier for biotechs and pharmas to patent phages,” she says.
But Hatfull and his team haven’t paused to bask in the limelight. They have already identified another two phages for Isabelle, in case she develops a resistance to the current cocktail, and they’re seeking phages for other patients, too. Meanwhile, the Hatfull lab is exploring how to battle the causative agent of tuberculosis, which infects approximately one-third of the world’s population and is responsible for roughly 1.5 million deaths per year.
He cautions people not to expect phages to replace antibiotics. But the two therapies might become complementary partners in brand new cocktails, perhaps ones designed to prevent the emergence of superbugs in the first place.
It’s easier than ever to stay motivated in his research, he says, because now he can recall how he felt when he saw Isabelle playing with her family’s dog in her backyard during a recent TV interview.
“This is a kid who we didn’t expect to survive,” he says.
And with that, he gets back to work.
Cover image: Graham Hatfull
This article appeared in the Fall 2019 edition of Pitt Magazine.