Jim and Martha Funderburgh stood in an operating room in 2014, suited up in surgical scrubs. The two researchers were in the Indian city of Hyderabad, waiting for a moment that was decades in the making. In just a few minutes, they would watch as a colleague performed the first operation using a technique they helped develop—a technique that can restore vision to damaged eyes.
The procedure would take less than 10 minutes, but it has the potential to bring a sea change to more than 6 million people around the world who suffer from corneal blindness. The only way to reverse this condition used to be through transplantation—removing the impaired cornea and replacing it with one from a deceased donor. The quicker, more elegant solution, pioneered at Pitt, offers the chance to rescue sight in a safer, more affordable way.
Later, Sayan Basu, the ophthalmologist who performed the operation, would tell Jim that he had a name for the procedure: “The Funderburgh Technique.” Jim politely declined the offer. It’s been a team effort to get this far, he explained. And the path there was illuminated, in part, by his wife, Martha.
She was in her early twenties when she woke up with a strange tingle in her right eye. Soon, the tingling evolved into a painful sore. Doctors identified the problem as ocular herpes, a recurrent virus that causes cold sore-like lesions on the eye and annually affects more than 50,000 people in the United States. Over the years, she was warned, the condition would lead to scarring on the cornea and a loss of vision.
The diagnosis was troubling, but it didn’t hold her back from her ambitions, which included the pursuit of a career in science. It was something she shared with her husband, Jim Funderburgh. Martha would go on to earn a master’s degree in public health, and Jim, fascinated by the fundamental elements of the body, would earn a PhD in physiological chemistry. Although Martha’s corneal disease never slowed her studies, it did influence the course of the Funderburghs’ careers.
Almost a decade after Martha’s diagnosis, Jim made a fortuitous connection with Martha’s ophthalmologist at the University of Washington. The eye expert explained to him the worldwide impact of corneal disease the likes of Martha’s and the imperfect treatment options available. Jim accepted a postdoctoral position studying corneal disease in the ophthalmologist’s lab, and through that job, he found his calling.
“The cornea is a living window to the world,” Jim says. A transparent outer layer that covers the iris and pupil, it’s responsible for helping the eye focus by bending, or refracting, light. “I became really fascinated with it as an important component of the visual system and also as a useful experimental system for understanding cell biology.”
He eventually established a lab at Kansas State University to study the cornea. Martha, her eyesight progressively diminishing, taught biology at the college and later channeled her scientific curiosity into her own career in ocular research alongside Jim.
By her early forties, however, her vision had diminished significantly. When it got so bad that she could no longer coach youth soccer, she knew that the only option to restore her vision was to undergo corneal transplantation.
Stem cells are a basic building block of the body and a core component of regenerative medicine. They can be converted to generate specialized cells that perform different jobs, like building bone, regrowing heart muscle—or forming the cornea. It’s believed that they lead to more successful outcomes when used as alternatives to transplantation, because the body is less likely to reject them.
Each year, more than 40,000 corneal transplants are performed in the United States, and about half fail within 10 years. Martha is lucky—the transplants she received are still going strong. Her vision is now “pretty good,” she says, though she still takes daily medication to limit complications.
In thinking about the people who aren’t so fortunate, Jim’s inquisitive mind whirred. Could there be a better way to treat this kind of blindness?
The Funderburghs arrived at the University of Pittsburgh in 1999, drawn by the opportunity to translate Jim’s research into potential treatments. He was named associate director of the Louis J. Fox Center for Vision Restoration, a nationally regarded comprehensive research and clinical program dedicated to ocular regenerative medicine. There, Jim established the Corneal Cell Biology Lab. Martha, with decades of corneal research under her belt, serves as lab manager.
The researchers went to work investigating alternatives to corneal transplants. They started by brainstorming what type of tissue could mimic a donated cornea. Efforts to grow corneal cells in the lab weren’t panning out—they couldn’t get them to create the transparent tissue that makes up the cornea.
Then, in a seminar in 2002 at Pitt’s McGowan Institute for Regenerative Medicine, the scientists learned that most tissues in the body harbor stem cells. A light bulb suddenly turned on.
“We could grow these stem cells and then convert them into corneal cells,” Jim remembers realizing.
In other words, they could use adult stem cells to regrow a healthy cornea.
Stem cells are a basic building block of the body and a core component of regenerative medicine. They can be converted to generate specialized cells that perform different jobs, like building bone, regrowing heart muscle—or forming the cornea. It’s believed that they lead to more successful outcomes when used as alternatives to transplantation, because the body is less likely to reject them.
Martha set to work with donor tissue, looking for stem cells near the cornea that had the potential to become corneal cells. In 2005, she found them. Over the following years, the Funderburghs and their colleagues in the lab learned to differentiate stem cells into functional corneal cells.
For the first time, these cells could make transparent corneal tissue in a laboratory dish. When the tissue was implanted into an animal eye, it remained transparent, just as it should. The solution wasn’t perfect, though: the tissue wasn’t strong or thick enough to be a substitute for a human cornea. The lab began to explore ways to produce a bigger, stronger, bioengineered cornea.
“Then the idea occurred to us: Maybe we don’t have to build a whole new tissue,” Jim says. “Maybe we can just put those stem cells directly into an eye and they would fix the scarring problem. To which everyone kind of rolled their eyes and said, ‘Yeah, right.’”
Amazingly, however, it worked. When injected into the cornea, the stem cells produced healthy corneal tissue. More importantly, in the presence of stem cells, the vision-reducing, opaque scar tissue gradually disappeared and was replaced by normal, transparent corneal tissue.
“I believe that the stem cells may be activating a potential present in our body that allows organs to regenerate on their own,” explains Jim. “We are very focused on finding more about this ‘biological switch’ that might control our ability to regenerate damaged tissue. Being able to induce our own bodies to heal themselves would transform medicine.”
The research was published in the journal Stem Cells. It took years of hard work to get there, but it was just the beginning.
In 2011, Jim Funderburgh had just finished delivering a presentation on his lab’s findings to an international conference when he and his team made a connection that would expand the possibilities of their work. They were approached by Virender Singh Sangwan, a professor and ophthalmologist from the L V Prasad Eye Institute in Hyderabad, India.
“We were saying that stem cell therapy was working really well and we were kind of wondering where to go with this,” Martha says. “And he said, ‘We’ve got a million people who need this.’”
 With Sangwan was Sayan Basu, an ophthalmologist and cornea specialist. He often saw corneal damage from injuries or illnesses in his practice, but donor corneas in India are in short supply. He hoped to learn more about how stem cells might be able to help his patients.
With Sangwan was Sayan Basu, an ophthalmologist and cornea specialist. He often saw corneal damage from injuries or illnesses in his practice, but donor corneas in India are in short supply. He hoped to learn more about how stem cells might be able to help his patients.
From within the sterile operating room, the Funderburghs watched as Basu delicately worked on the patient, a woman with corneal scarring that had impaired her vision—just like what Martha had once experienced. He gave her local anesthesia before gently removing the outer layer of the corneal cells. He then spread on a dab of gel that contained the patient’s own stem cells mixed with a protein that would work to heal the scarring and restore sight.
Basu soon came to Pittsburgh to study at the Corneal Cell Biology Lab. Between 2012 and 2013, he learned laboratory techniques and how to culture stem cells—information he took back with him to Hyderabad, where he set up his own lab.
But Basu also helped advance the Pitt lab’s research.
In India, he had developed a technique called limbal biopsy, where stem cells can be extracted from a patient’s own eye using an incisional biopsy. There, he used it for the treatment of corneal burns. But in Pittsburgh, he wondered if the practice could be used in place of Jim’s way of getting stem cells—through donor tissue. Basu tried it out, wondering if the limbal biopsy stem cells would be comparable to those taken from donor tissue. They were.
It was a breakthrough. Now they didn’t have to negotiate the severe shortage of donor tissue. Eye banks in the United States sent more than 26,000 corneas overseas in 2016 to those awaiting transplants, according to the Eye Bank Association of America. Yet, in India at least 120,000 people are blind and 6.8 million people have visual impairment because of corneal damage. Basu’s findings, made in collaboration with the Pitt team, were published in the journal Science Translational Medicine and would help pave the way to future clinical work in patients.
While working with Basu, Jim Funderburgh had his own breakthrough. He developed a way to paste the stem cells onto the eye in a kind of gel, rather than injecting them. It simplified the procedure and made it safer.
After returning to Hyderabad, Basu started a series of trials to treat corneal damage in humans using stem cells applied in gel. Then, in 2014, Jim and Martha traveled to the L V Prasad Eye Institute in India to witness that first-ever procedure.
From within the sterile operating room, the Funderburghs watched as Basu delicately worked on the patient, a woman with corneal scarring that had impaired her vision—just like what Martha had once experienced. He gave her local anesthesia before gently removing the outer layer of the corneal cells. He then spread on a dab of gel that contained the patient’s own stem cells mixed with a protein that would work to heal the scarring and restore sight. After placing a bandage-like contact lens over the area, the operation was complete. It took mere minutes.
Basu conducted a pilot trial and a clinical trial in which Jim was a collaborator and senior investigator. Over 70 patients have been treated with the technique so far, with no reported complications and a high rate of vision improvement. They are waiting for patients to complete their one-year follow-up and for regulatory authorities to approve publishing. The interim analysis of the results, Basu says, is “extremely encouraging.”
Through the Funderburghs’ ongoing research, exciting new treatment options in ophthalmology are in sight.
“The initial results of the ongoing trial in India lay the basis for a much larger therapeutic program that has the potential to cure or prevent blindness in a significant number of patients worldwide,” says José-Alain Sahel, the chair of the Department of Ophthalmology at Pitt’s School of Medicine and director of the UPMC Eye Center. “This would be the culmination of an amazing scientific career demonstrating the importance of unwavering, steady pursuit of a line of research over decades, from cell biology to molecular mechanisms and clinical translation. This, alongside the human values that Martha and Jim illustrate every day, sets a standard for our department’s future.”
They aren’t the kind of people to rest on their laurels, however.
“I think I am just a born scientist,” Jim says. “I like to investigate and discover stuff.”
To that end, the work coming out of his lab continues to explore new facets of potential treatments, often through multidisciplinary collaboration. One particular partnership has emerged from Pitt’s School of Dental Medicine, where Fatima Syed-Picard, an assistant professor, has conducted research indicating that stem cells extracted from wisdom teeth can be used to regenerate the cornea. The finding presents the possibility that adult stem cells may soon become more accessible.
As he looks to the future, Jim wants to make restoring corneal damage even easier and more convenient for people in need around the globe.
“Can we get a way to deliver these cells that doesn’t mean the doctor’s office has to be across the hall from the cell culture lab?” he asks. “Can we get these to people around the world?”
Funding from the United States Department of Defense is helping the lab answer those questions. With it, the researchers have developed a collagen-like stem cell bandage that could be administered to wounded service members in the case that a blast or other trauma burns their cornea. The study with their finding was recently published in Stem Cells Translational Medicine.
Meanwhile, the researchers are exploring options of using either the stem cells or the products made by the cells in clinical trials in the United States. Though the process is slow and expensive, Jim is hopeful that they could have a product ready for initial clinical trials within the next two years.
It’s an exciting outlook for a research team inspired by personal experience and driven by the desire to help others see a brighter future.
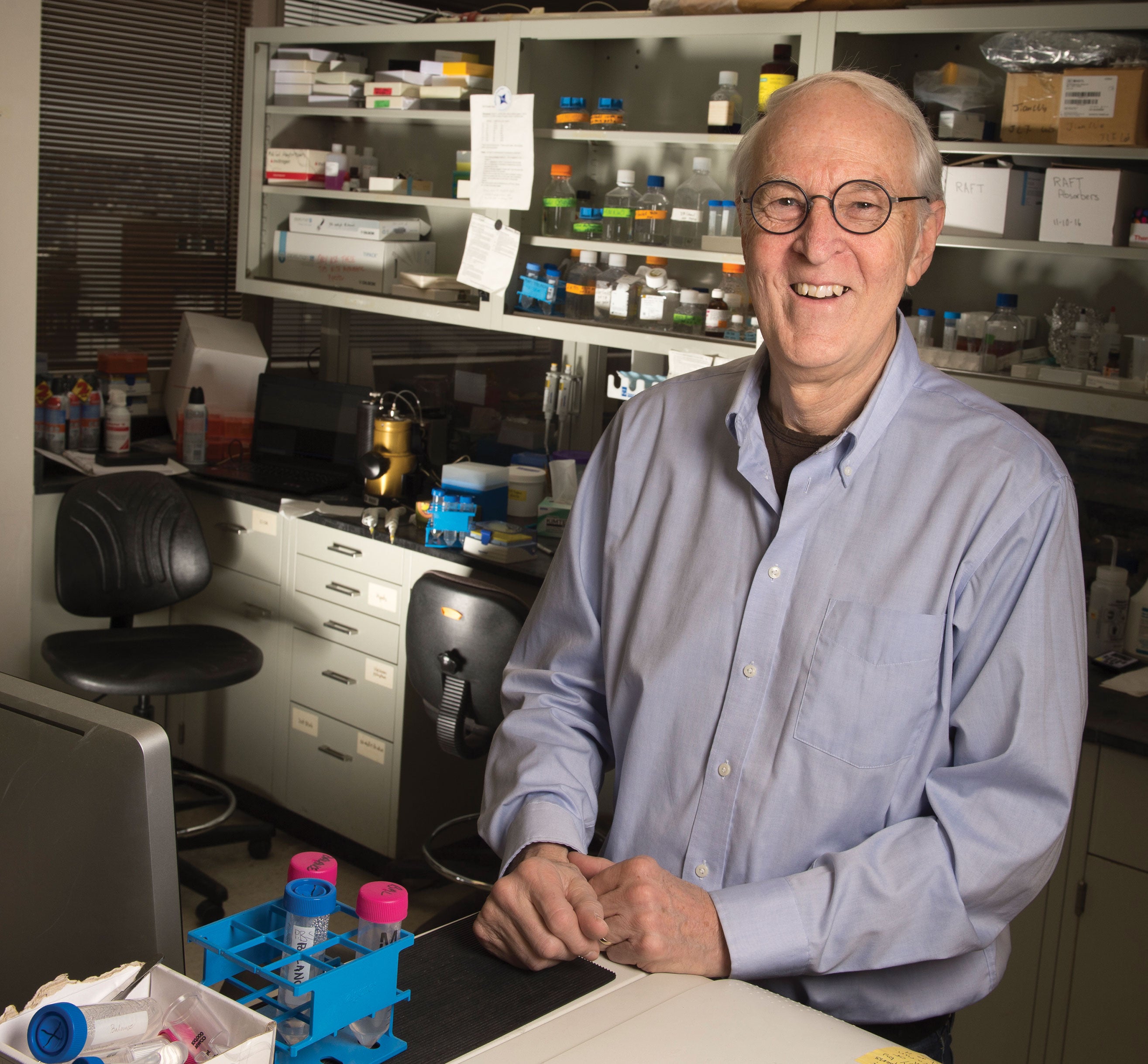
Opening image: Jim and Martha Funderburgh
This article appeared in the Summer 2018 issue of Pitt Magazine.





